Your Recovery
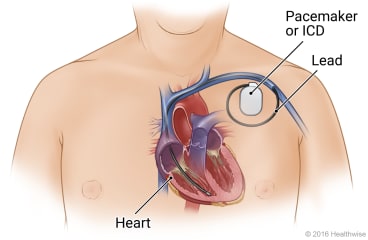
Pacemaker placement is surgery to put a pacemaker in your chest. This surgery may be done if you have bradycardia (a slow heart rate). Your doctor made a cut (incision) in your chest. The doctor put the pacemaker leads through the cut, into a large blood vessel, then into the heart. The doctor put the pacemaker under the skin of your chest and attached the leads to it.
Your chest may be sore where the doctor made the cut. You also may have a bruise and mild swelling. These symptoms usually get better in 1 to 2 weeks. You may feel a hard ridge along the incision. This usually gets softer in the months after surgery. You may be able to see or feel the outline of the pacemaker under your skin.
You may be able to go back to work or your usual routine 1 to 2 weeks after surgery. But for at least a few weeks after the surgery, you will avoid vigorous physical activity that involves your upper body.
Pacemaker batteries may last about 10 years. If the battery gets low, you will need to decide whether to have another surgery to replace the pacemaker.
You'll need to take steps to safely use electric devices. Some of these devices can stop your pacemaker from working right for a short time. Check with your doctor about what to avoid and what to keep a short distance away from your pacemaker. For example, you will need to stay away from things with strong magnetic and electrical fields. An example is an MRI machine (unless your pacemaker is safe for an MRI). You can use a cell phone and other wireless devices, but keep them at least 6 inches away from your pacemaker. Many household and office electronics don't affect a pacemaker.
This care sheet gives you a general idea about how long it will take for you to recover. But each person recovers at a different pace. Follow the steps below to get better as quickly as possible.
How can you care for yourself at home?
 Activity
Activity
- Rest when you feel tired.
- Be active. Walking is a good choice.
- Do not raise your arm (on the side of your body where the pacemaker is located) above shoulder level until your doctor says it's okay. This helps keep the pacemaker and leads in place while you heal. Your doctor may recommend gentle range-of-motion exercises for your shoulder.
- For at least 3 or 4 weeks, or for as long as your doctor says, avoid activities that strain your chest or upper arm muscles. This includes mopping floors or pushing a lawn mower or vacuum. It also includes swinging a golf club or tennis racquet or swimming.
- You may need to take about 1 to 2 weeks off from work. It depends on the type of work you do and how you feel.
- Ask your doctor when you can drive again.
- Ask your doctor when it is okay for you to have sex.
 Diet
Diet
- You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
 Medicines
Medicines
- Your doctor will tell you if and when you can restart your medicines. The doctor will also give you instructions about taking any new medicines.
- If you stopped taking aspirin or some other blood thinner, your doctor will tell you when to start taking it again.
- Be safe with medicines. Read and follow all instructions on the label.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- Do not take aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), or other nonsteroidal anti-inflammatory drugs (NSAIDs) unless your doctor says it is okay.
 Incision care
Incision care
- If you have strips of tape on the incision, leave the tape on for a week or until it falls off.
- You may shower 24 to 48 hours after surgery. Pat the incision dry. Don't swim or take a bath for the first 2 weeks or until your doctor tells you it is okay.
- You will have a dressing over the incision. A dressing helps the incision heal and protects it. Your doctor will tell you how to take care of this.
 Other instructions
Other instructions
- Keep a medical ID card with you at all times that says you have a pacemaker. The card should include the manufacturer and model information.
- Wear medical alert jewelry stating that you have a pacemaker. You can buy this at most drugstores.
- Tell all of your doctors, dentists, and other health professionals that you have a pacemaker before you have any test, procedure, or surgery.
- Ask your doctor for a list of electric devices that you might need to keep a short distance from your pacemaker.
- Check your pulse as directed by your doctor.
- Have your pacemaker checked as often as your doctor recommends. In some cases, this may be done from your home. Your doctor will give you instructions about how to do this.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
When should you call for help?
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have trouble breathing.
Call your doctor now or seek immediate medical care if:
- You are dizzy or light-headed, or you feel like you may faint.
- You have pain that does not get better after you take pain medicine.
- You hear an alarm or feel a vibration from your pacemaker.
- You have loose stitches, or your incision comes open.
- Bright red blood has soaked through the bandage over your incision.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
- You have hiccups often or for a long time.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You have any problems with your pacemaker.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter G550 in the search box to learn more about "Pacemaker Placement: What to Expect at Home".
Current as of: October 2, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

