Overview
Chronic obstructive pulmonary disease (COPD) is a lung disease that makes it hard to breathe.
COPD is usually caused by smoking. It is also caused by air pollution. Other things that may lead to COPD include breathing chemical fumes, factory dust, soot, and secondhand smoke over a long period of time.
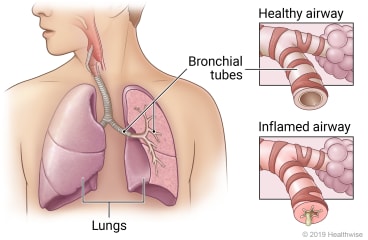
Chronic bronchitis and emphysema are two lung problems that are types of COPD. In chronic bronchitis, the airways that carry air to the lungs (bronchial tubes) get inflamed and make a lot of mucus. This can narrow or block the airways, making it hard for you to breathe. It can also make you cough. In emphysema, the air sacs in your lungs are damaged and lose their stretch. Less air gets in and out of your lungs, which makes you feel short of breath.
Treatment can help you feel better and prevent symptoms from getting worse quickly. Some treatments may also slow the disease and help you live longer.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
How can you care for yourself at home?
Staying healthy
- If you smoke, try to quit or cut back as much as you can. Not smoking is the most important step you can take to slow the disease and help you feel better. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- Try to avoid infections such as COVID-19, colds, and the flu. Wash your hands often. You may want to wear a mask when you go to public indoor places. Try to avoid sick people.
- Stay up to date on vaccines. Get the pneumococcal and whooping cough (pertussis) vaccines. If you have had these vaccines before, ask your doctor if you need another dose. Get the flu vaccine every year. Stay up to date on your COVID-19 vaccines. Get the shingles vaccine. Ask your doctor if the RSV (respiratory syncytial virus) vaccine is right for you.
- Try to avoid things that could make your symptoms worse. These include secondhand smoke, chemical fumes, factory dust, soot, and air pollution. Talk to your doctor about ways to protect yourself if you are exposed to substances that irritate your lungs at home or at work.
- Watch for changes in your symptoms. If they get worse over a short time and stay bad, it's called a flare-up. Your doctor can help you make a plan so you know what to do and take action.
- Take care of your teeth and gums. Get regular dental checkups.
Medicines and oxygen therapy
- Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
- You will get more details on the specific medicines your doctor prescribes. Medicines can help you breathe easier and feel better. Medicines can help prevent flare-ups and may also help you live longer.
- Ask your doctor, pharmacist, or respiratory therapist how to use each of your inhalers correctly. With correct use, the medicine is more likely to get to your lungs.
- Ask your doctor, pharmacist, or respiratory therapist if a spacer is right for you. A spacer may help you get more inhaled medicine to your lungs. If you use one, ask how to use it properly.
- Do not take any vitamins, over-the-counter medicine, or herbal products without talking to your doctor first.
- If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
- If you use oxygen therapy, use the flow rate your doctor has recommended. Don't change it without talking to your doctor first. Oxygen therapy boosts the amount of oxygen in your blood and helps you breathe easier.
 Activity
Activity
- Try to be active every day. Being as active as you can may help you feel better and may help prevent problems. For many people, walking is a good choice. Or you may want to swim, bike, or do other activities.
- Pay attention to your breathing. You are exercising too hard if you can't talk while you exercise.
- If your doctor has not set you up with a pulmonary rehabilitation program, ask if rehab is right for you. Rehab can help relieve your shortness of breath and improve your quality of life. Rehab includes exercise programs, education about your disease and how to manage it, help with diet and other changes, and emotional support.
- Try to conserve, or save, your energy when you do daily activities. For example, take short rest breaks when doing household chores. Ask your doctor or pulmonary rehabilitation team for tips that may help you feel less tired and have more energy.
- Learn breathing methods that help you slow down and control your breathing. These methods include pursed lip breathing or belly breathing. Use these methods when you are more short of breath than usual. Practice them often so you can use them correctly when you need to.
 Diet
Diet
- Try to eat regular, healthy meals.
- Use bronchodilators about 1 hour before you eat to make it easier to eat.
- Try ways to avoid shortness of breath while eating. For example, eat several smaller, frequent meals to prevent getting too full. A full stomach can push on the muscle that helps you breathe (your diaphragm) and make it harder to breathe.
- Drink beverages at the end of the meal so you don't feel too full during the meal.
- Talk with your doctor if you need help staying at a weight that's healthy for you.
- Talk with your doctor if you lose weight without trying. Your doctor and a dietitian can help you make a plan to get enough calories and protein to maintain your weight.
Mental health
- Tell your doctor if you feel sad, depressed, or hopeless. Also tell your doctor if you have lost interest in things you usually enjoy or if you have been nervous, worried, or on edge. If needed, medicine and counseling can help.
- Seek connections. Spend time with friends, family, and others. Joining a support group for people with COPD may help.
When should you call for help?
Call 911 anytime you think you may need emergency care. For example, call if:
- You have severe trouble breathing.
- You have severe chest pain.
Call your doctor now or seek immediate medical care if:
- You have new or worse trouble breathing.
- You have new or worse chest pain.
- You cough up blood.
- You have a fever.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You cough more deeply or more often, especially if you notice more mucus or a change in the color of your mucus.
- You have new or worse swelling in your legs or belly.
- You have feelings of anxiety or depression.
- You need to use your antibiotic or steroid pills.
- You are not getting better as expected.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter X915 in the search box to learn more about "Chronic Obstructive Pulmonary Disease (COPD): Care Instructions".
Current as of: September 29, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

