What is pancreatitis?
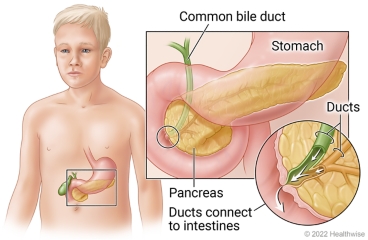
The pancreas is an organ behind the stomach. It makes hormones and enzymes to help the body digest food.
Usually these enzymes flow from the pancreas to the intestines. But if they leak into the pancreas, they can irritate it and cause pain and swelling. This is called pancreatitis.
Pancreatitis often happens suddenly (acute). It lasts a short time. Most children have one attack and get better.
Sometimes a child gets pancreatitis more than once (acute recurrent). Or it turns into a long-term (chronic) condition. These problems are rare in children.
What causes it?
Pancreatitis is often caused by gallstones. These are stones that form in the gallbladder. They can block the tubes (ducts) that drain into the intestines.
Other causes may include:
- A problem with how the pancreas or ducts are formed.
- Some medicines that treat long-term health problems.
- An injury to the belly.
- Infections (like mumps).
- High levels of fats in the blood.
In many cases, doctors may not know the cause.
What are the symptoms?
The main symptom of pancreatitis is pain or tenderness in the upper part of the belly. The pain can be severe. In older children, the pain can spread to their back. Babies and very young children may be cranky and cry more.
Your child may also have a fever, nausea, or vomiting. Not all children will have all these symptoms.
Some children get so sick that they have problems breathing.
Children with chronic pancreatitis may have other symptoms too. These include slow growth, weight loss, belly pain after eating, diarrhea, and oily stools. The stools may float in the toilet bowl.
How is it diagnosed?
Your child's doctor will do an exam. The doctor will ask about your child's symptoms and past health. The doctor may be able to tell that your child has this problem based on the symptoms and where the child has pain in the belly.
Your child may have blood tests. These tests will check the levels of enzymes called amylase and lipase. With this condition, the levels of these enzymes are often very high.
Your child also may have imaging tests of the belly. These may include an ultrasound or MRI. Sometimes a special MRI test is used to look for blocked ducts.
How is it treated?
Treatment includes taking care of symptoms and supporting your child's body while the pancreas heals. This care may happen at a hospital.
Your child may get medicine to ease the pain and nausea. Fluids may be given through a vein (I.V.). Your child can start eating as soon as they feel ready. For severe cases, your child may be fed through a feeding tube or an I.V. until they can eat by mouth.
If gallstones are causing the problem, the doctor may do a procedure to remove the stones.
Children with chronic pancreatitis might need to eat a low-fat diet and take enzyme pills. They may use pain medicine. In rare cases, surgery is needed if medicine doesn't help ease the pain.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter A122 in the search box to learn more about "Learning About Pancreatitis in Children".
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

