What is a hemodialysis access?
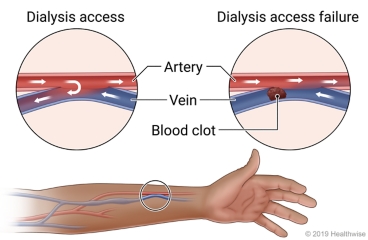
A hemodialysis access is a site on your body where dialysis needles can be placed. It's most often made by joining a vein and an artery, usually in an arm. Your blood flows through the needles and into tubes that go to and from a dialysis machine to remove wastes from your blood.
What causes it to fail?
Several things can cause a vascular access to fail. They include:
- Infection.
- Blood clots in the access.
- Bleeding from the access.
- A buildup of fluid or blood around the access.
- Narrowing of the blood vessels in or around the access.
- Blood vessels that are blocked, such as by a blood clot.
- Use of devices that can slow blood flow. Examples are catheters, pacemakers, and defibrillator leads.
An access can sometimes fail before it has been used the first time.
How is access failure diagnosed?
Access failure is often found by the dialysis nurse during a treatment session. The nurse may notice that dialysis or the access is not working as well as it should.
If your doctor suspects access failure, you will need a physical exam. This may include checking your access for a vibration, called a thrill. Your doctor may also check it for a swishing sound, called a bruit (say "BROO-ee"). These are signs that your access is working.
The doctor may also looks for signs of infection, such as swelling, warmth, or redness in the area. Your doctor may also look at the color and temperature of your hands and arms.
You may get tests. These can include blood tests. You may also get imaging tests of your blood vessels, such as Doppler ultrasound or angiogram.
How is it treated?
When a vascular access fails, your doctor needs to quickly repair or replace it. It has to work well so you can keep up with your dialysis sessions.
- If blood flow is blocked, your doctor may be able to clear it with a tiny balloon or tube (stent). Sometimes a blood clot can be cleared with blood thinner medicine.
- If your access is infected, you will get antibiotic medicine.
- If your access needs time to heal, you will have a tunneled catheter for dialysis. You'll have this for a few weeks until your permanent access works again.
- If you need a new permanent access, talk to your doctor about your options.
How can you prevent vascular access failure?
It's important to take care of your vascular access so that it works well. Any access has some risk of failure. So follow these tips to protect your access.
- Do not lift anything heavy with your access arm.
- Do not bump your access arm.
- Don't wear tight clothing or jewelry over that arm.
- Don't sleep with your access arm under your body.
- Do not have blood drawn or blood pressure measured on your access arm.
- Don't put cream or lotion on or near the access.
- Keep the area clean and dry.
- Tell your health care team right away if you notice anything unusual in how your access looks or feels.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter H005 in the search box to learn more about "Learning About Hemodialysis Vascular Access Failure".
Current as of: October 11, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

