What are blood transfusions?
Blood transfusion is a medical treatment to replace the blood or parts of blood that your child's body has lost. The blood goes through a tube from a bag to an intravenous (I.V.) catheter and into your child's vein.
Your child may need a blood transfusion after losing blood from an injury, a major surgery, an illness that causes bleeding, or an illness that destroys blood cells.
Transfusions are also used to give your child the parts of blood. These may include platelets, plasma, or substances that cause clotting. These may be needed if your child's body needs to fight an illness or stop bleeding.
How is a blood transfusion done?
Before your child receives a blood transfusion, their blood is tested to find out what type it is. Blood or blood parts that are a match with your child's blood type are ordered by the doctor. Blood is typed as A, B, AB, or O. It is also typed as Rh-positive or Rh-negative.
Your child's blood is also screened to look for antibodies that might react with the blood that is given to your child. The blood your child gets is checked and rechecked to make sure that it's the right type.
A sample of your child's blood is mixed with a sample of the blood they will receive. This is done to check for problems. Before giving the transfusion, a doctor or nurse will look at the label on the package of blood and compare it to your child's hospital ID bracelet and medical records. The transfusion begins only when all agree that this is the correct blood and that your child is the correct person to receive it.
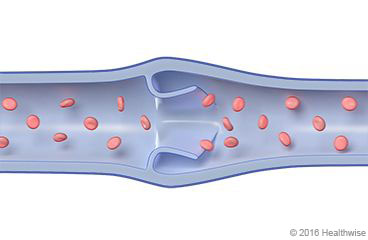
To receive the transfusion, your child will have an intravenous (I.V.) catheter inserted into a vein. A tube connects the catheter to the bag containing the blood, which is placed higher than your child's body. The blood then flows slowly into your child's vein. A doctor or nurse will check your child several times during the transfusion to watch for a reaction or other problems.
What are the possible risks?
Blood transfusions have many benefits and are often life-saving. But they also have a few risks. Possible risks include:
- Your body's reaction to receiving new blood. This may include:
- Fever.
- Breathing problems.
- Allergic reaction, such as hives, swelling, or a new rash.
- An infection from the blood. This risk is small because of the strict rules placed on handling and storing blood. Getting a viral infection, such as HIV or hepatitis B or C, through blood transfusions has become very rare. The U.S. Food and Drug Administration (FDA) enforces strict guidelines on the collection, testing, storage, and use of blood.
- Getting the wrong blood type by accident. Severe reactions, which can be life-threatening, are very rare.
- An infection at the transfusion site, such as redness, swelling, pain, bleeding, or pus.
How can you care for your child at home?
To prevent infection at the transfusion site
- Wash the area daily with warm, soapy water, and pat it dry. Don't use hydrogen peroxide or alcohol, which can slow healing. You may cover the area with a gauze bandage if it weeps or rubs against clothing. Change the bandage every day.
- Keep the area clean and dry.
When should you call for help?
Call 911 anytime you think your child may need emergency care. For example, call if:
- Your child has severe trouble breathing. (Your child can't talk at all.) Young children may have flared nostrils, and their belly moves in and out with every breath.
- Your child passes out (loses consciousness) or is very hard to wake up.
Call your doctor now or seek immediate medical care if:
- Your child has new or worse trouble breathing.
- Your child is dizzy or lightheaded or seems like they may faint.
- Your child has a fever or chills.
- Your child has chest pain, back pain, or pain in the flank, which is just below the rib cage and above the waist on either side of the back.
- Your child has blood in their urine.
- Your child has abnormal bleeding, such as:
- Nosebleeds.
- New bleeding or oozing at an intravenous (I.V.) or blood draw site.
- Your child has little to no urine when they try to urinate.
- Your child has belly pain, nausea, vomiting, or diarrhea.
- Your child has signs of an allergic reaction, such as hives, swelling, or a new rash.
- Your child has signs of an infection at the transfusion site, such as redness, swelling, pain, bleeding, or pus.
- Your child seems weaker or more tired than usual.
- Your child has a yellow tint (jaundice) to their skin or the whites of the eyes.
Watch closely for changes in your child's health, and be sure to contact your doctor if your child has any problems.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter C381 in the search box to learn more about "Learning About Blood Transfusions in Children".
Current as of: October 7, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

