Overview
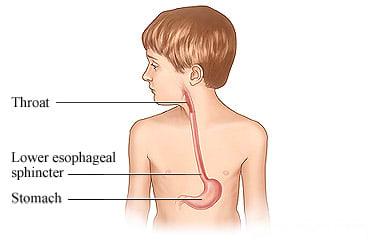
Gastritis is an upset stomach. It happens when something irritates the stomach lining. Many things can cause gastritis, such as an infection or illness, food or drink, or medicines. Your child's belly may bloat and ache. Your child may belch, vomit, and feel sick to their stomach.
Minor stomach upset can be treated at home. Medicines that reduce or block stomach acid may help. If gastritis lasts, your doctor may prescribe medicine.
Follow-up care is a key part of your child's treatment and safety. Be sure to make and go to all appointments, and call your doctor if your child is having problems. It's also a good idea to know your child's test results and keep a list of the medicines your child takes.
How can you care for your child at home?
- Have your child take medicines exactly as prescribed. Call your doctor if you think your child is having a problem with a medicine.
- Note when your child gets an upset stomach. Write down any foods, medicines, or events that seem to cause stomach upset. Avoid these in the future.
- Do not give your child over-the-counter medicines without talking to your doctor first. Do not give Pepto-Bismol or other medicines that contain salicylates, a form of aspirin.
- Watch for and treat signs of dehydration, which means that the body has lost too much water. Your child's mouth may feel very dry. Your child may have sunken eyes with few tears when crying. Your child may lack energy and want to be held a lot. And your child may not urinate as often as usual.
- Give your child lots of fluids a little at a time. This is very important if your child is vomiting or has diarrhea. Give your child sips of water or drinks such as Pedialyte or Infalyte. These drinks contain a mix of salt, sugar, and minerals. You can buy them at drugstores or grocery stores. Give these drinks as long as your child is throwing up or has diarrhea. Do not use them as the only source of liquids or food for more than 12 to 24 hours.
- Avoid foods that make your child's symptoms worse. These may include chocolate, mint, alcohol, pepper, spicy foods, high-fat foods, or drinks with caffeine in them, such as tea, coffee, colas, or energy drinks.
- Start to offer small amounts of food when your child feels like eating.
When should you call for help?
Call 911 anytime you think your child may need emergency care. For example, call if:
- Your child passes out (loses consciousness).
- Your child is confused, does not know where they are, or is extremely sleepy or hard to wake up.
- Your child has severe belly pain.
- Your child vomits blood or what looks like coffee grounds.
- Your child passes maroon or very bloody stools.
Call your doctor now or seek immediate medical care if:
- Your child has new or worse belly pain.
- Your child has a new or higher fever.
- Your child has symptoms of dehydration, such as:
- Dry eyes and a dry mouth.
- Passing only a little urine.
- Feeling thirstier than usual.
- Your child has nausea or vomiting and can't keep medicine or fluids down.
- Your child cannot pass stools or gas.
- Your child has new or more blood in their stools or their stools are black and tarlike.
Watch closely for changes in your child's health, and be sure to contact your doctor if:
- Your child has new symptoms, such as a rash, an earache, or a sore throat.
- Your child does not get better as expected.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter G537 in the search box to learn more about "Gastritis in Children: Care Instructions".
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

