Overview
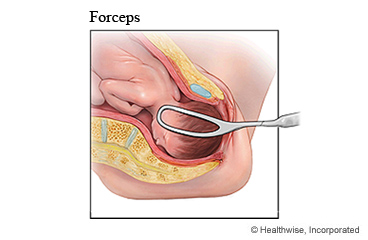
Sometimes a baby needs a little help when coming through the birth canal during delivery. When this happens, the doctor may use forceps to help deliver the baby. This is called a forceps-assisted delivery. Forceps look like a long pair of spoons or tongs.
Before a forceps delivery, the vagina and the area around it are numbed with an anesthetic. A cut (incision) may be made to make the opening of the vagina bigger. Then the doctor gently places the forceps on either side of the baby's head and turns the baby or pulls the baby out.
Your body will slowly heal in the next few weeks.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
How can you care for yourself at home?
Vaginal bleeding and cramps
- After delivery, you will have a bloody discharge from the vagina. This will turn pink within a week and then white or yellow after about 10 days. It may last for 2 to 4 weeks or longer, until the uterus has healed. Use sanitary pads until you stop bleeding. Using pads makes it easier to monitor your bleeding.
- Do not worry if you pass some blood clots, as long as they are smaller than a golf ball. If you have a tear or stitches in your vaginal area, change the pad at least every 4 hours to prevent soreness and infection.
- You may have cramps for the first few days after childbirth. These are normal and occur as the uterus shrinks to normal size. Take an over-the-counter pain medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve), for cramps. Read and follow all instructions on the label. Do not take aspirin, because it can cause more bleeding.
- Do not take two or more pain medicines at the same time unless the doctor told you to. Many pain medicines have acetaminophen, which is Tylenol. Too much acetaminophen (Tylenol) can be harmful.
Stitches
- If you have stitches, they will dissolve on their own and do not need to be removed. Follow your doctor's instructions for cleaning the stitched area.
- Put ice or a cold pack on the painful area for 10 to 20 minutes at a time, several times a day, for the first few days. Put a thin cloth between the ice and your skin.
- Sit in a few inches of warm water (sitz bath) 3 times a day and after bowel movements. The warm water helps with pain and itching. If you do not have a tub, a warm shower might help.
Breast fullness
- Your breasts may overfill (engorge) in the first few days after delivery. To help milk flow and to relieve pain, warm your breasts in the shower or by using warm, moist towels before nursing.
- If you are not nursing, do not put warmth on your breasts or touch your breasts. Wear a bra that fits well and use ice until the fullness goes away. This usually takes 2 to 3 days.
- Put ice or a cold pack on your breast after nursing to reduce swelling and pain. Put a thin cloth between the ice and your skin.
 Activity
Activity
- Eat a balanced diet. Do not try to lose weight by cutting calories. Keep taking your prenatal vitamins, or take a multivitamin.
- Get as much rest as you can. Try to take naps when your baby sleeps during the day.
- Get some exercise every day. But do not do any heavy exercise until your doctor says it is okay.
- Wait until you are healed (about 4 to 6 weeks) before you have sexual intercourse. Your doctor will tell you when it is okay to have sex.
- If you don't want to get pregnant, talk to your doctor about birth control. You can get pregnant even before your period returns. Also, you can get pregnant while you are breastfeeding.
Mental health
- It is normal to have some sadness, anxiety, sleeplessness, and mood swings after you go home. If you feel upset or hopeless for more than a few days or are having trouble doing the things you need to do, talk to your doctor.
Constipation and hemorrhoids
- Drink plenty of fluids. If you have kidney, heart, or liver disease and have to limit fluids, talk with your doctor before you increase the amount of fluids you drink.
- Eat plenty of fiber each day. Have a bran muffin or bran cereal for breakfast, and try eating a piece of fruit for a mid-afternoon snack.
- For painful, itchy hemorrhoids, put ice or a cold pack on the area several times a day for 10 minutes at a time. Follow this by putting a warm compress on the area for another 10 to 20 minutes or by sitting in a shallow, warm bath.
When should you call for help?
Share this information with your partner, family, or a friend. They can help you watch for warning signs.
Call 911 anytime you think you may need emergency care. For example, call if:
- You feel you cannot stop from hurting yourself, your baby, or someone else.
- You passed out (lost consciousness).
- You have chest pain, are short of breath, or cough up blood.
- You have a seizure.
Where to get help 24 hours a day, 7 days a week
If you or someone you know talks about suicide, self-harm, a mental health crisis, a substance use crisis, or any other kind of emotional distress, get help right away. You can:
- Call the Suicide and Crisis Lifeline at 988.
- Call 1-800-273-TALK (1-800-273-8255).
- Text HOME to 741741 to access the Crisis Text Line.
Consider saving these numbers in your phone.
Go to 988lifeline.org for more information or to chat online.
Call your doctor or midwife now or seek immediate medical care if:
- You have signs of hemorrhage (too much bleeding), such as:
- Heavy vaginal bleeding. This means that you are soaking through one or more pads in an hour. Or you pass blood clots bigger than an egg.
- Feeling dizzy or lightheaded, or you feel like you may faint.
- Feeling so tired or weak that you cannot do your usual activities.
- A fast or irregular heartbeat.
- New or worse belly pain.
- You have signs of infection, such as:
- A fever.
- Increased pain, swelling, warmth, or redness from an incision or wound.
- Frequent or painful urination or blood in your urine.
- Vaginal discharge that smells bad.
- New or worse belly pain.
- You have symptoms of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in the calf, back of the knee, thigh, or groin.
- Swelling in the leg or groin.
- A color change on the leg or groin. The skin may be reddish or purplish, depending on your usual skin color.
- You have signs of preeclampsia, such as:
- Sudden swelling of your face, hands, or feet.
- New vision problems (such as dimness, blurring, or seeing spots).
- A severe headache.
- You have signs of heart failure, such as:
- New or increased shortness of breath.
- New or worse swelling in your legs, ankles, or feet.
- Sudden weight gain, such as more than 2 to 3 pounds in a day or 5 pounds in a week.
- Feeling so tired or weak that you cannot do your usual activities.
- You had spinal or epidural pain relief and have:
- New or worse back pain.
- Increased pain, swelling, warmth, or redness at the injection site.
- Tingling, weakness, or numbness in your legs or groin.
Watch closely for changes in your health, and be sure to contact your doctor or midwife if:
- Your vaginal bleeding isn't decreasing.
- You feel sad, anxious, or hopeless for more than a few days.
- You are having problems with your breasts or breastfeeding.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter Z892 in the search box to learn more about "Forceps-Assisted Delivery: Care Instructions".
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

