This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
Childhood Stomach Cancer
Childhood stomach cancer is a very rare cancer that starts in the cells lining the stomach. The stomach is an organ on the left side of the upper abdomen that digests food. The stomach is part of the digestive tract, a series of hollow, muscular organs joined in a long, twisting tube from the mouth to the anus. The digestive tract processes nutrients in foods that are eaten and helps pass waste material out of the body:
- Food moves from the throat to the stomach through a tube called the esophagus.
- After food enters the stomach, it is broken down by stomach muscles that mix the food and liquid with digestive juices.
- After leaving the stomach, partly-digested food passes into the small intestine and then into the large intestine.
- The end of the large intestine, called the rectum, stores the waste from the digested food until it is pushed out of the anus during a bowel movement.
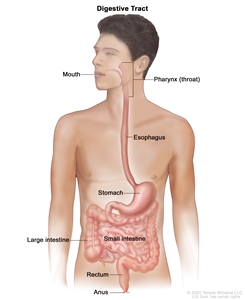
Anatomy of the digestive tract. The digestive tract is made up of organs that food and liquids travel through when they are swallowed, digested, absorbed, and leave the body as feces. These organs include the mouth, pharynx (throat), esophagus, stomach, small intestine, large intestine, rectum, and anus.
Causes and risk factors for childhood stomach cancer
Childhood stomach cancer is caused by certain changes to the way stomach cells function, especially how they grow and divide into new cells. Often, the exact cause of the cell changes is unknown. To learn more about how cancer develops, see What Is Cancer?
A risk factor is anything that increases the chance of getting a disease. Not every child with a risk factor will develop stomach cancer, and it will develop in some children who don't have a known risk factor.
Risk factors for childhood stomach cancer include:
- H. pylori infection. Chronic infection of the mucosal layer of the stomach with H. pylori is a risk factor for stomach cancer. This bacterium spreads from person to person through direct contact with saliva, vomit, or stool. Although many people with chronic H. pylori infections do not have symptoms, some develop stomach ulcers or inflammation of the stomach called atrophic gastritis. In some people, atrophic gastritis leads to increasingly severe changes in the stomach lining and eventually to stomach cancer or gastric MALT lymphoma. Treatment of H. pylori infections reduces the risk of these types of stomach cancer. To learn more, see H. pylori and cancer.
- Hereditary diffuse gastric cancer (HDGC). HDGC is a rare, inherited type of stomach cancer caused by a mutation (change) in the CDH1 gene. To learn more, see HDGC.
Talk with your child's doctor if you think your child might be at risk of stomach cancer.
Genetic counseling for children with stomach cancer
It may not be clear from the family medical history whether a child with stomach cancer has an inherited condition that increased their risk. Genetic testing may help explain why a child develops a rare cancer or a cancer that is usually seen in adults, such as stomach cancer. Genetic counselors and other specially trained health professionals can discuss your child's diagnosis and your family's medical history to help you understand:
- your options for CDH1 gene testing for hereditary diffuse gastric cancer
- the risk of other cancers for your child
- the risk of stomach cancer and other cancers for your child's siblings
- the risks and benefits of learning genetic information
Genetic counselors can also help you cope with your child's genetic testing results, including how to discuss the results with family members.
Symptoms of childhood stomach cancer
Many children do not have symptoms of stomach cancer until the cancer has spread. It's important to check with your child's doctor if your child has any symptoms below:
- stomach pain
- loss of appetite
- weight loss for no known reason
- nausea
- vomiting
- constipation or diarrhea
- weakness
- anemia (symptoms of which may include tiredness, dizziness, fast or irregular heartbeat, shortness of breath, and pale skin)
These symptoms may be caused by conditions other than childhood stomach cancer. The only way to know is to see your child's doctor. The doctor will ask you when the symptoms started and how often your child has been having them as a first step in making a diagnosis.
Diagnosis of childhood stomach cancer
If your child has symptoms that suggest stomach cancer, the doctor will need to find out if they are due to cancer or another condition. The doctor will ask about your child's personal and family medical history and do a physical exam. Depending on these results, they may recommend tests to find out if your child has stomach cancer.
The following tests and procedures are used to diagnose stomach cancer. The results will also help you and your child's doctor plan treatment.
CT scan (CAT scan)
A CT scan uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
To learn more, see Computed Tomography (CT) Scans and Cancer.
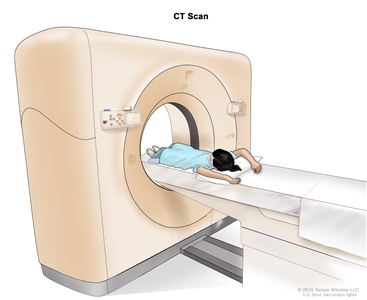
Computed tomography (CT) scan. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of areas inside the body.
Upper endoscopy with biopsy
Upper endoscopy is a procedure to look inside the esophagus, stomach, and duodenum (first part of the small intestine) to check for abnormal areas. An endoscope is passed through the mouth and down the throat into the esophagus. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples (biopsy), which are checked under a microscope for signs of cancer.
The sample of tissue may be used for biomarker testing.
Talk with your child's doctor about what to expect during and after your child's biopsy.
To learn about the type of information that can be found in a pathologist's report about the cells or tissue removed during a biopsy, see Pathology Reports.
Barium swallow
Barium swallow is a series of x-rays of the esophagus and stomach. The patient drinks a liquid that contains barium (a silver-white metallic compound). The liquid coats the esophagus and stomach, and x-rays are taken. This procedure is also called an upper GI series.
Getting a second opinion
You may want to get a second opinion to confirm your child's stomach cancer diagnosis and treatment plan. If you seek a second opinion, you will need to get important medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans before giving a recommendation. The doctor who gives the second opinion may agree with the first doctor, suggest changes or another approach, or provide more information about your child's cancer.
To learn more about choosing a doctor and getting a second opinion, see Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital that can provide a second opinion. For questions you might want to ask at your appointments, see Questions to Ask Your Doctor about Cancer.
Prognostic factors for childhood stomach cancer
If your child has been diagnosed with stomach cancer, you may have questions about how serious the cancer is and your child's chances of survival. The likely outcome or course of a disease is called prognosis. The prognosis can be affected by whether the cancer has spread to other parts of the body at the time of diagnosis and how well the cancer responds to treatment. Your child's oncology care team is in the best position to talk with you about your child's prognosis.
Stages of childhood stomach cancer
Cancer stage describes the extent of cancer in the body, such as the size of the tumor, whether it has spread, and how far it has spread from where it first formed. There is no staging system used for childhood stomach cancer, but the tests and procedures done to diagnose the cancer are also used to help plan treatment.
Types of treatment for childhood stomach cancer
There are different types of treatment for children and adolescents with stomach cancer. You and your child's cancer care team will work together to decide treatment. Many factors will be considered, such as your child's overall health and whether the cancer is newly diagnosed or has come back.
A pediatric oncologist, a doctor who specializes in treating children with cancer, will oversee treatment. The pediatric oncologist works with other pediatric health professionals who are experts in treating children with cancer and who specialize in certain areas of medicine. This may include the following specialists and others:
- pediatrician
- pediatric gastroenterologist
- pediatric surgeon
- radiation oncologist
- pathologist
- pediatric nurse specialist
- social worker
- rehabilitation specialist
- psychologist
- child-life specialist
- fertility specialist
Your child's treatment plan will include information about the cancer, the goals of treatment, treatment options, and the possible side effects. It will be helpful to talk with your child's cancer care team before treatment begins about what to expect. For help every step of the way, see our downloadable booklet, Children with Cancer: A Guide for Parents.
Surgery
Surgery to remove the tumor is the main treatment for stomach cancer.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. Stomach cancer is sometimes treated with external beam radiation therapy. This type of radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Radiation therapy may be given alone or with other treatments, such as chemotherapy.
To learn more, see External Beam Radiation Therapy for Cancer and Radiation Therapy Side Effects.
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Chemotherapy may be given alone or with other types of treatment, such as radiation therapy.
For stomach cancer, the chemotherapy is injected into a vein. When given this way, the drugs enter the bloodstream to reach cancer cells throughout the body. Chemotherapy drugs used to treat stomach cancer in children are
Combinations of these drugs may be used. Other chemotherapy drugs not listed here may also be used.
To learn more about how chemotherapy works, how it is given, common side effects, and more, see Chemotherapy to Treat Cancer.
Clinical trials
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. Because cancer in children is rare, taking part in a clinical trial should be considered.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Some clinical trials are open only to patients who have not started treatment. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more, see Clinical Trials Information for Patients and Caregivers.
Treatment of childhood stomach cancer
Treatment of newly diagnosed stomach cancer in children may include:
- surgery to remove the cancer and some healthy tissue around it
- surgery to remove as much of the cancer as possible, followed by radiation therapy and chemotherapy
If your child's cancer comes back after treatment, their doctor will talk with you about what to expect and next steps. There might be treatment options that may shrink the cancer or control its growth. If there are no treatments, your child can receive care to control symptoms from cancer so they can be as comfortable as possible.
Side effects of treatment
To learn more about side effects that begin during treatment for cancer, see Side Effects.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include the following:
- physical problems
- changes in mood, feelings, thinking, learning, or memory
- second cancers (new types of cancer) or other conditions
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the possible late effects caused by some treatments.
Learn more about Late Effects of Treatment for Childhood Cancer.
Follow-up testing
Some of the tests that were done to diagnose the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has recurred (come back). These tests are sometimes called follow-up tests or check-ups.
Coping with cancer
When your child has cancer, every member of the family needs support. Honest and calm conversations build trust as you talk with your child and their siblings. Taking care of yourself during this difficult time is also important. Reach out to your child's treatment team and to people in your family and community for support. To learn more, see Support for Families When a Child Has Cancer and the booklet Children with Cancer: A Guide for Parents.
Last Revised: 2024-04-11
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

