Your Recovery
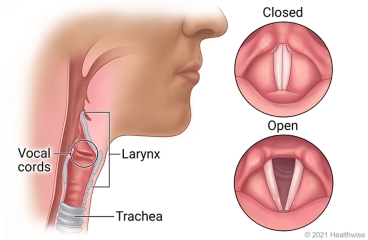
Laryngectomy is the removal of all or part of the voice box (larynx). The voice box is in the neck and contains the vocal cords. It also helps you swallow and breathe.
After surgery, the area around the cut (incision) may be swollen or bruised. It may also feel numb. This is common and may continue for a few weeks. You will probably need to take pain medicine for a few weeks.
You may have a drain tube in your neck for 1 to 4 days after your surgery. You may have trouble swallowing for several days after you go home. Also, you may have numbness in your neck and weakness in your face. Most of this goes away in 3 to 4 months.
For 2 to 3 weeks, you will either get food through a tube that goes into your nose and down your throat to your stomach, or through a tube that goes directly into your stomach. Your doctor will give you detailed information on what and how you can eat using the feeding tube.
Your ability to talk will depend on how much of your voice box was removed. If all of it was removed, you will need to learn new ways to communicate. If only a part of your voice box was removed, you may be able to talk after your throat has healed. Losing your ability to talk can be very upsetting and hard to accept. It can affect your self-image and lead to depression. If you need help after surgery, you may want to consult with a counselor.
If all of your voice box was removed, you will have a hole in your neck to help you breathe. This is called a stoma. A doctor or nurse will teach you how to care for the stoma.
Most people go back to work or to their normal routine 6 to 8 weeks after going home. You will need more time to get better if you must have more treatment for cancer, such as chemotherapy.
This care sheet gives you a general idea about how long it will take for you to recover. But each person recovers at a different pace. Follow the steps below to get better as quickly as possible.
How can you care for yourself at home?
 Activity
Activity
- Rest when you feel tired. Getting enough sleep will help you recover. Sleep with your head up by using three or four pillows. You can also try to sleep with your head up in a reclining chair. Do not sleep on your stomach.
- Try to walk each day. Start by walking a little more than you did the day before. Bit by bit, increase the amount you walk. Walking boosts blood flow and helps prevent pneumonia and constipation. You may climb stairs.
- Be careful while showering and shaving if you have a stoma in your neck. Do not get water in the stoma, because it could get into your lungs. If you have a stoma, follow your doctor's instructions on how to care for it.
- Do not lean your head back quickly or for a long time. This puts pressure on your neck and may slow your healing.
- Avoid strenuous activities, such as bicycle riding, jogging, weight lifting, or aerobic exercise, until your doctor says it is okay. This includes mowing the lawn or shoveling snow.
- For about 6 weeks, avoid lifting anything that would make you strain. This may include a child, heavy grocery bags and milk containers, a heavy briefcase or backpack, cat litter or dog food bags, or a vacuum cleaner.
- Ask your doctor when you can drive again.
 Diet
Diet
- Your diet will go from a clear liquid diet, to a full liquid diet, and then a soft diet before you can eat normally. This generally takes 1 to 2 months. Most people are on a soft diet when they leave the hospital. Your doctor will give you specific information about what you can eat.
- If you are on a soft diet, eat foods that are easy to swallow and digest. These include pancakes and waffles; most cereals; scrambled eggs and omelets; canned or cooked fruits; finely ground beef, chicken, turkey, and pork; mild cheeses; potatoes and pasta; and cooked vegetables.
- It is important to keep your weight and energy up. Do not fill up your stomach with sweets like candy and cookies. Sweets may also make you feel lightheaded and cause a problem called dumping syndrome. Dumping syndrome can make you feel faint, bloated, shaky, and sick to your stomach. It also can cause diarrhea.
- Sit up straight when you eat and for 30 to 60 minutes after you are done eating. This can help food move through your digestive tract. Try not to eat anything in the 3 hours before you go to bed.
- You may notice that your bowel movements are not regular right after your surgery. This is common. Try to avoid constipation and straining with bowel movements. You may want to take a fiber supplement every day. If you have not had a bowel movement after a couple of days, ask your doctor about taking a mild laxative.
 Medicines
Medicines
- Your doctor will tell you if and when you can restart your medicines. The doctor will also give you instructions about taking any new medicines.
- If you stopped taking aspirin or some other blood thinner, your doctor will tell you when to start taking it again.
- Be safe with medicines. Take pain medicines exactly as directed.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- If you think your pain medicine is making you sick to your stomach:
- Take your medicine after meals (unless your doctor has told you not to).
- Ask your doctor for a different pain medicine.
- Your doctor may prescribe antibiotics. Take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
 Incision care
Incision care
- If you have strips of tape on the incision, leave the tape on for a week or until it falls off.
- Wash the area daily with warm, soapy water and pat it dry. Your doctor will tell you how to take care of this. Don't use hydrogen peroxide or alcohol, which can slow healing. You may cover the area with a gauze bandage if it weeps or rubs against clothing. Change the bandage every day.
 Other instructions
Other instructions
- If you have a stoma, keep it covered with a light cloth. This keeps out dust and particles that could enter your lungs and cause problems.
- You may want to use a humidifier to add moisture to the air. This keeps the stoma from drying out and getting crusty. Follow the directions for cleaning the machine.
- It is normal to have some yellowish mucus around your feeding tube. This is not a sign of infection. Keep your feeding tube clamped unless you are using it. Keep it taped to your skin at all times. Be sure there is some slack in the tube so if you move suddenly, it does not pull out.
- If you cannot talk after surgery, a speech therapist will teach you new ways to communicate.
- Find a counselor you like and trust if you are having trouble coping after surgery.
Follow-up care is a key part of your treatment and safety. Be sure to make and go to all appointments, and call your doctor if you are having problems. It's also a good idea to know your test results and keep a list of the medicines you take.
When should you call for help?
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have sudden chest pain and shortness of breath, or you cough up blood.
- You have severe trouble breathing.
Call your doctor now or seek immediate medical care if:
- You have pain that does not get better after you take pain medicine.
- You have blood leaking from your incision.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
Watch closely for any changes in your health, and be sure to contact your doctor if:
- You are not getting better as expected.
Where can you learn more?
Go to http://www.healthwise.net/patientEd
Enter I060 in the search box to learn more about "Laryngectomy: What to Expect at Home".
Current as of: October 27, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.

