Cigna Healthcare PPO Network Providers providing urgent or emergency care outside of Kaiser Permanente's service state (California, Colorado, District of Columbia, Georgia, Hawaii, Maryland, Oregon, Virginia, and Washington) should contact Kaiser Permanente as soon as possible for Cigna precertification questions, eligibility verification, and benefits verification at Kaiser Permanente's dedicated phone line for Cigna Healthcare PPO providers: 888.831.0761.
Provider information

Provider Details for an HMO, EPO, & POS 2-Tier Member
Effective August 1, 2022, Kaiser Permanente members with HMO (health maintenance organization) or participating EPO (exclusive provider organization) plans began to have access to emergency and urgent care services at Cigna Healthcare negotiated rates via Cigna Healthcare’s PPO (preferred provider organization) Network* of providers when traveling outside Kaiser Permanente states (California, Colorado, District of Columbia, Georgia, Hawaii, Maryland, Oregon, Virginia, and Washington) and if applicable, no payment is required from eligible members until after the claim is priced by Cigna Healthcare and paid by Kaiser Permanente.
Similarly, effective October 1, 2022, the above became applicable to Kaiser Permanente Point of Service (POS) 2-Tier members began to have access to emergency and urgent care services at Cigna Healthcare negotiated rates via Cigna Healthcare’s Preferred Provider Organization (PPO) Network* of providers when traveling outside of Kaiser Permanente states.
The Cigna Healthcare PPO Network refers to the health care providers (doctors, hospitals, specialists) contracted as part of the Cigna Healthcare PPO for Shared Administration.
What this means to Cigna Healthcare PPO Network Providers
Cigna Healthcare PPO Network providers outside of Kaiser Permanente States will be reimbursed for qualifying for urgent or emergency care services they provide to eligible Kaiser Permanente (HMO, EPO, POS 2-Tier) members and should not collect cost share from eligible Kaiser Permanente members upfront once benefits/eligibility is determined.
Cigna Healthcare providers are to send their urgent or emergency care claims for HMO, EPO, & POS 2-Tier members from ALL KP regions (excluding Washington) to:
Cigna Medical Claims
P.O. Box 188061
Chattanooga, TN 37422-8061
Payer ID 62308
Please send your claims appeal or payment dispute to: California - Northern. Please send your claims appeal or payment dispute to:
- California - Northern
| Authorized Services | Emergency Services |
|---|---|
| Kaiser Referral Invoice Center (RISC) 2829 Watt Avenue, Suite #130 Sacramento, CA 95821 |
Kaiser Foundation Health Plan, Inc. Claims Administration Department Attn: Provider Dispute Services Unit P.O. Box 23100 Oakland, CA 94623 |
- California – Southern
Kaiser Foundation Health Plan, Inc.
California Claims Administration
Post Office Box 7006
Downey, CA 90242-7006
- Colorado
Kaiser Permanente Colorado – Provider Appeals
Claims Administration Department
ATTN: Provider Appeals
PO Box 373150
Denver, CO 80237-1750
- Georgia
Kaiser Permanente Georgia – Provider Appeals
Claims Administration Department
ATTN: Provider Appeals
PO Box 370010
Denver, CO 80237-9998
- Hawaii
Kaiser Permanente Hawaii – Provider Appeals
Claims Administration Department
ATTN: Provider Appeals
PO Box 378021
Denver, CO 80237-9998
- Mid-Atlantic States
Kaiser Permanente MAS - Provider Appeals
Claims Administration Department
ATTN: Provider Appeals
P.O. Box 371860
Denver CO 80237-9998
Fax: 855-414-2622
- Northwest
Kaiser Permanente Northwest – Provider Appeals
Claims Administration Department
ATTN: Provider Appeals
PO Box 370050
Denver, CO 80237-9998
- All Regions Self-Funded Plans
Kaiser Permanente Insurance Company
Claims Administrator
P.O. Box 30547
Salt Lake City, UT 84130-0547
EDI Payor ID # 94320
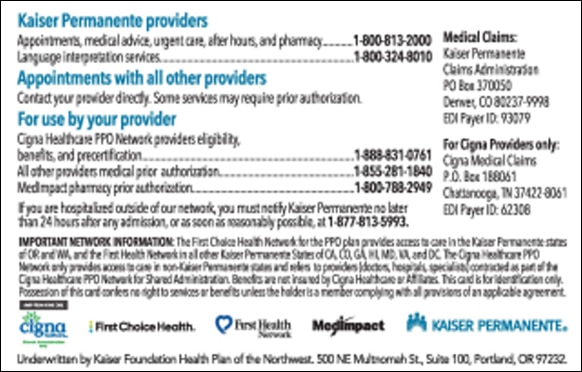
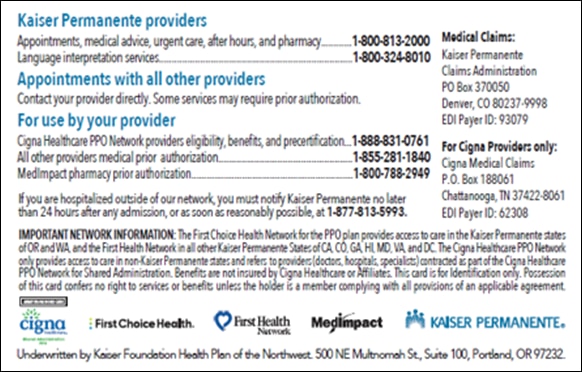
Cigna Healthcare providers can easily identify Kaiser Permanente patients by checking their Kaiser Permanente Digital ID card or their new travel card:
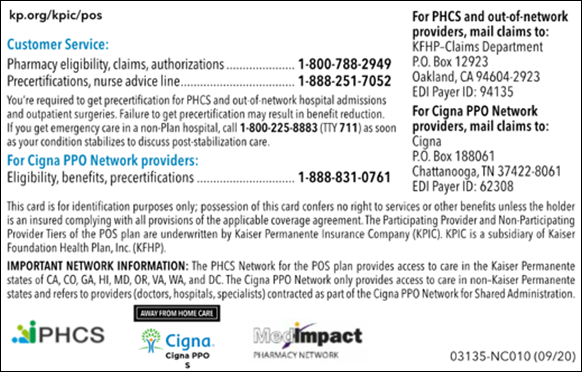
- For eligible members, the back of their updated digital ID card says:
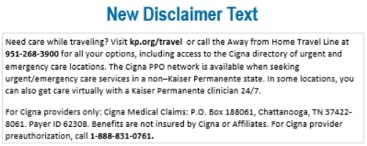
Note: Text on the digital ID card disclaimer is subject to change
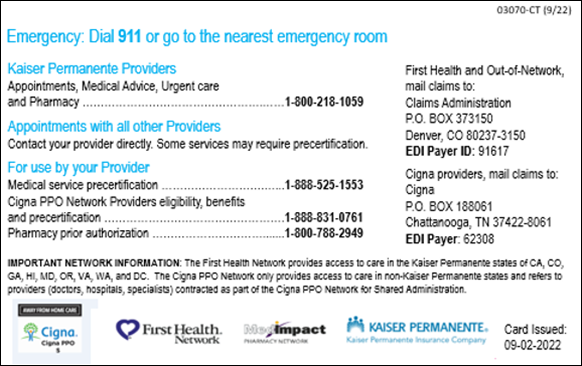
Show their new travel card which they will start receiving in late-November. For eligible members, the back of their new Travel ID card says:
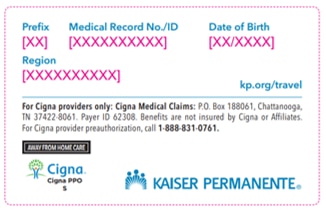
Note: Text on the physical Travel ID card is subject to change
Members who are unable to present either form of verification may be verified eligible by calling 888.831.0761
Provider Details for an PPO, & 3-Tier POS Member
Effective January 1, 2023, Kaiser Permanente Insurance Company (KPIC) PPO and Kaiser Permanente’s 3-Tier POS members began to have access to most covered services including outpatient and inpatient services, but not limited to, emergency and urgent care services via Cigna Healthcare’s PPO network of physicians, hospitals, and urgent care clinics while outside of a Kaiser Permanente states (California, Colorado, District of Columbia, Georgia, Hawaii, Maryland, Oregon, Virginia, and Washington). Additionally, this change became effective January 1, 2024, for Oregon situs members enrolled in PPO and 3-Tier POS coverage issued by Kaiser Foundation Health Plan of Northwest.
The Cigna Healthcare PPO Network refers to the health care providers (doctors, hospitals, specialists) contracted as part of the Cigna Healthcare PPO for Shared Administration.
What this means to Providers in Cigna Healthcare’s PPO network:
Cigna Healthcare PPO Network providers outside of Kaiser Permanente States will be reimbursed for qualifying services they provide to eligible Kaiser Permanente (3-Tier POS) or KPIC (PPO) members and should only collect applicable cost share from eligible Kaiser Permanente 3-Tier POS or KPIC PPO members upfront once benefits/eligibility is determined.
(Reimbursement based on Cigna Healthcare reimbursement policies and provider’s Cigna Healthcare PPO agreement)
- Cigna Healthcare providers are to send their claims for PPO and 3-Tier POS members from ALL KP regions (except Northwest & Washington) to:
Cigna Medical Claims
P.O. Box 188061
Chattanooga, TN 37422-8061
Payer ID 62308
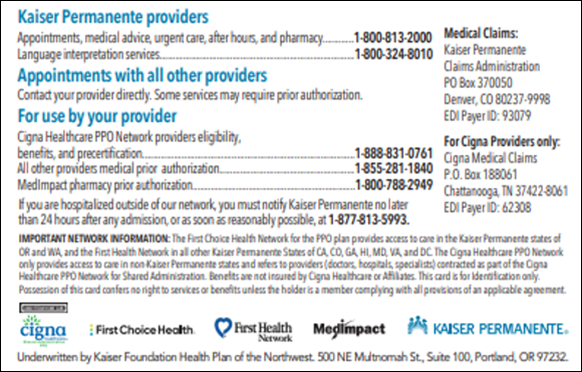
Cigna Healthcare providers can easily identify Kaiser Permanente or Kaiser Permanente Insurance Company patients by checking their Kaiser Permanente Physical ID card or Digital ID card.
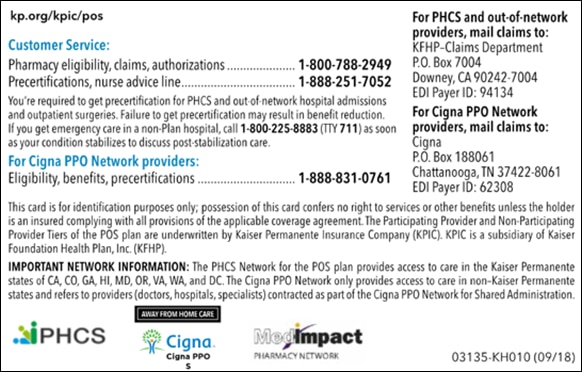
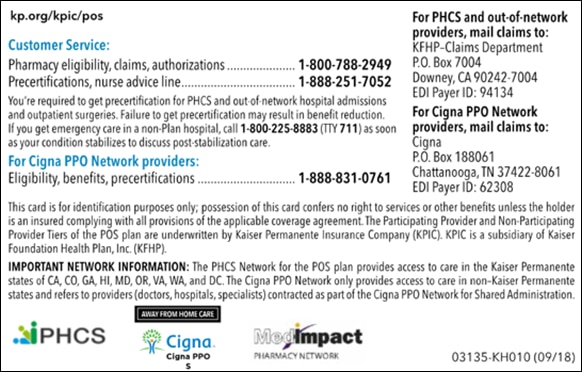
For eligible members, the back of their new ID card says:
Note: Text on the physical ID card is subject to change
- SCAL POS:
- SCAL PPO
- NCAL POS
- NCAL PPO
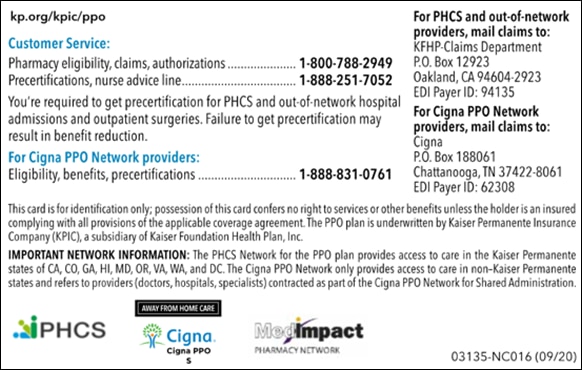
- CO POS
- CO PPO
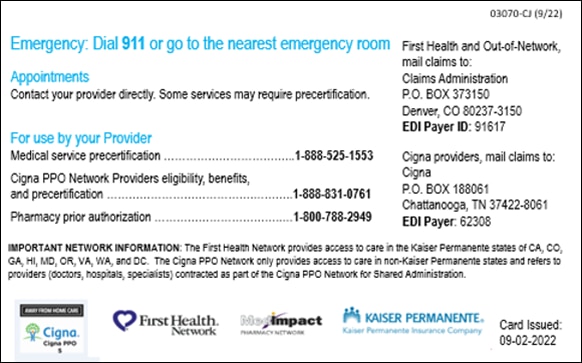
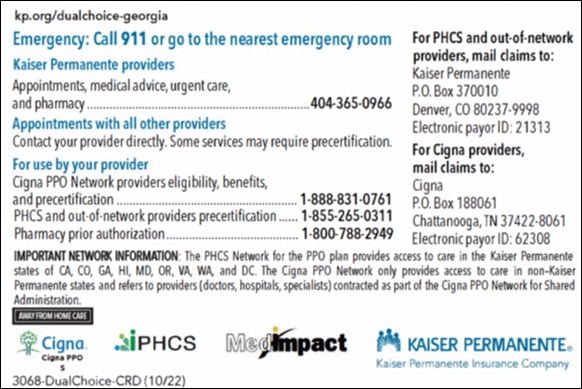
- GA Dual Choice PPO:
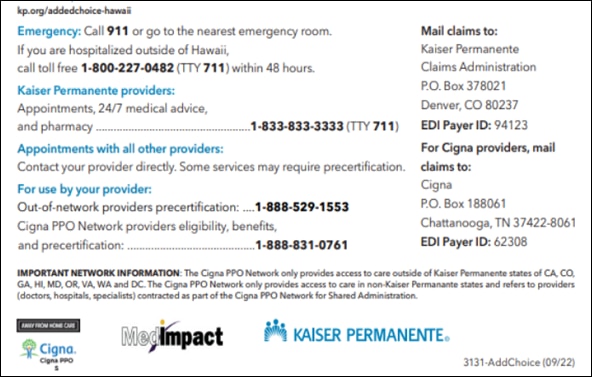
- HI Added Choice (3-Tier POS):
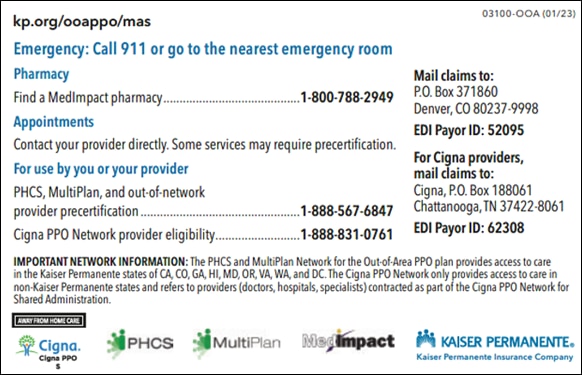
- MAS Out of Area PPO:
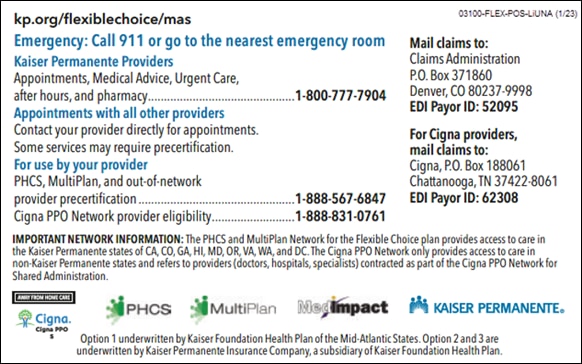
- MAS Flexible Choice (3-Tier POS):
- NW Oregon Added Choice (3-Tier POS):
- NW Oregon Dual Choice PPO:
- NW Oregon PPO Plus:
Members who are unable to present either form of verification may be verified eligible by calling 888.831.0761
*The Cigna Healthcare PPO Network refers to the health care providers (doctors, hospitals, specialists) contracted as part of the Cigna PPO for Shared Administration. Cigna Healthcare is an independent company and not affiliated with Kaiser Foundation Health Plan, Inc., and its subsidiary health plans. Access to the Cigna Healthcare PPO Network is available through Cigna Healthcare’s contractual relationship with the Kaiser Permanente health plans. The Cigna Healthcare PPO Network is provided exclusively by or through operating subsidiaries of Cigna Corporation, including Cigna Health and Life Insurance Company. The Cigna Healthcare name, logo, and other marks are owned by Cigna Intellectual Property, Inc.
**Eligibility Exceptions: The Cigna Healthcare PPO Network* enhanced experience for our members is not available to:
- HMO, EPO, PPO, & POS members enrolled in coverage issued by Kaiser Foundation Health Plan of Washington and Kaiser Foundation HealthPlan of Washington Options, Inc.
- PPO and POS 3-Tier members enrolled in coverage issued by Kaiser Foundation Health Plan of Northwest.
- Medicare members
- Medicaid members (Medi-Cal in California)
***Kaiser Permanente Insurance Company (KPIC) is a subsidiary of Kaiser Foundation Health Plan, Inc. (KFHP).